Government officials often portray themselves as champions of progress and stability, but the reality behind the NHS negotiations reveals a troubling disconnect. The recent standoff between the health secretary and the British Medical Association (BMA) exposes a government still struggling to comprehend the gravity of its workforce crisis. Instead of genuine empathy or strategic investment, there’s a reliance on superficial solutions that serve to delay undeniable reforms. The narrative constructed around local decision-making and incremental adjustments is a smokescreen that masks the core issue: a government unwilling, or perhaps incapable, of addressing the fundamental underfunding and undervaluation of medical professionals.
What fascinates—yet horrifies—about this situation is how political rhetoric is crafted to give an illusion of responsiveness while sidestepping meaningful change. Locally driven decisions may sound appealing on paper, but they risk further fragmenting an already strained system. Without a cohesive national strategy to restore fair salaries and working conditions, these piecemeal efforts merely delay the inevitable chaos. The government’s emphasis on ‘trust autonomy’ becomes a hollow gesture when the larger question remains unaddressed: why are NHS staff still fighting for basic pay restoration nearly two decades after they were first undercompensated?
The Fallacy of Public Support and the Real Cost of Negotiation Games
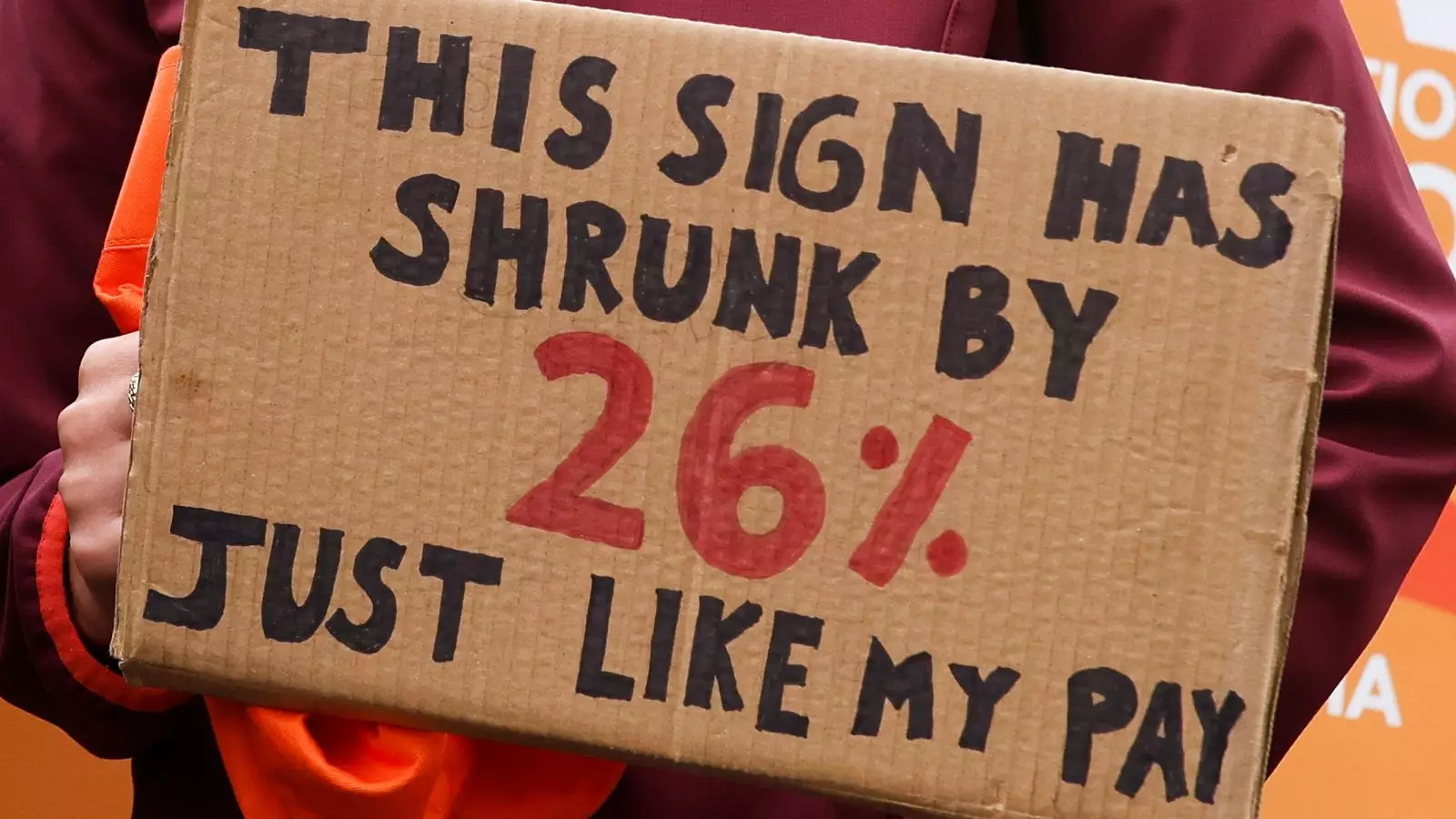
It’s tempting for policymakers to seize public opinion as a barometer of their success or failure, but in the case of NHS strikes, this approach oversimplifies a complex moral and social dilemma. The government’s framing—highlighting the recent 29% pay rise—ignores the nuances of inflation, cost of living increases, and the growing workload faced by resident doctors. The BMA’s demand for a 26% correction isn’t just about numbers; it’s about dignity, recognition, and survival in an underfunded system that has long undervalued its brightest frontline workers.
This discrepancy reveals a fundamental failure of political leadership. By fixating on optics—”look how much we’ve already given”—the government neglects the human cost. The public’s waning support for the strikes signals a broader societal fatigue with the endless cycle of concessions and stand-offs. It underscores a disconnect: voters are asked to accept a narrative of progress while frontline staff continue to endure the brunt of austerity measures, workplace burnout, and unsafe staffing levels.
The Dangerous Illusion of Decentralization as a Safety Net
Streeting’s proposal to delegate decisions to local trust leaders attempts to sidestep the deep-rooted issues through a decentralization strategy that may further jeopardize patient safety. The assumption is that local managers, who often lack the authority and resources to address systemic deficiencies, can make nuanced assessments that safeguard urgent care and protect vulnerable patients. This represents a shortsighted view—a fallback that shifts responsibility away from the core problem rather than tackles it head-on.
History shows that such decentralization often leads to uneven standards of care and a blame game where failures are diffused and factored into local budgets rather than addressed holistically. Patients, especially those battling deadly diseases like cancer, are collateral damage in this game of political brinkmanship. To suggest that a postponement of non-critical appointments can be a sustainable solution is a dangerous oversimplification that ultimately benefits no one except the political actors seeking to avoid confrontation.
The Deep-Rooted Problem: A Broken System and a Divided Workforce
The core issue lies in the systemic neglect that has persisted for over a decade. Underfunding, poor workforce planning, and a failure to value medical professionals have created a fragile NHS teetering on the brink of crisis. The resident doctors’ strike isn’t merely about pay; it’s a symptom of a healthcare system in dire need of overhaul—an overhaul the political establishment continues to resist, fearing the upheaval that real reform would entail.
Moreover, the state of public discourse around these strikes reveals a troubling tendency to pit patient safety against doctor demands—an artificial dichotomy that distracts from the real debate: how to rebuild and sustain a healthcare infrastructure capable of meeting future needs. When perceptions are infused with blame and short-term politicking, the long-term health of the NHS suffers. If the government persists in treating these disputes as political threats rather than opportunities for genuine reform, the consequences will resonate far beyond the current crisis.
Leave a Reply