For decades, the scientific consensus has relegated brain glycogen to a secondary position—an emergency reserve primarily stored in the liver and muscles, ready to be tapped during metabolic crises. This narrow view has limited our understanding of how critical energy management is within neural tissues, especially as we confront the growing prevalence of neurodegenerative diseases like Alzheimer’s. Emerging research, however, is tearing down this outdated paradigm, revealing that glycogen may play a far more dynamic and integral role in neuronal health and disease than previously imagined.
Recent findings indicate that glycogen accumulation in the brain isn’t just a benign energy store but may actively contribute to, or even drive, neurodegenerative pathology. This shift in perspective opens the door for novel intervention strategies that target the very foundation of neuronal energy regulation. The implications are profound, urging the scientific community—and society at large—to re-examine long-standing assumptions about brain metabolism and its influence on aging and disease.
The Hidden Connection Between Glycogen and Tau Pathology
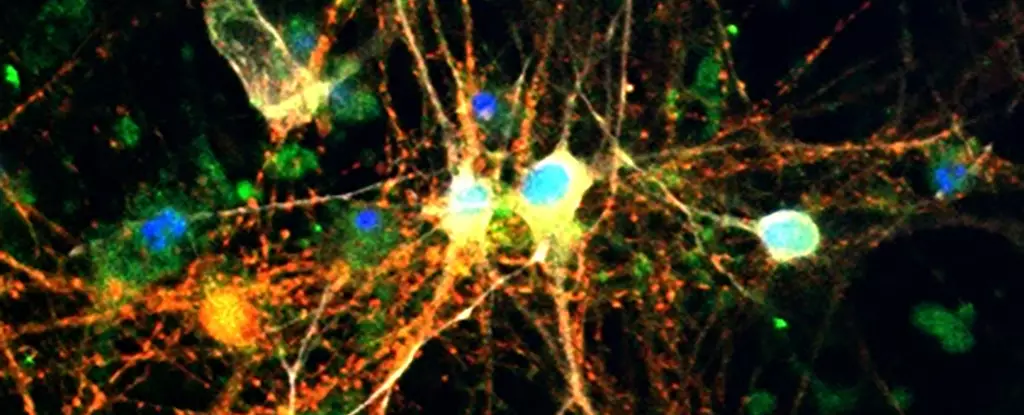
A pivotal aspect of this groundbreaking research lies in its exploration of the relationship between glycogen deposits and tau proteins—the molecular villains in Alzheimer’s disease. Traditionally, tau accumulation, or neurofibrillary tangles, has been viewed as a hallmark of disease progression, yet the root causes remain elusive. The new studies shed light on an intriguing interaction: excess glycogen levels are found in modeled models of tauopathies, both in genetically engineered fruit flies and in human brain tissues affected by Alzheimer’s.
What makes these findings particularly compelling is the mechanism uncovered by scientists. Tau proteins seem to disrupt the normal metabolic pathways that govern glycogen utilization, leading to harmful build-ups of both substances. This dual accumulation then exacerbates neuronal stress, diminishes the brain’s intrinsic defenses, and accelerates neurodegeneration. Here, the interaction between tau and glycogen isn’t merely a bystander effect but a potential catalyst that worsens disease severity.
Reimagining Therapeutic Approaches: The Role of Glycogen Phosphorylase
One of the most encouraging revelations from recent research is the potential to intervene directly in this maladaptive process. The enzyme glycogen phosphorylase (GlyP), responsible for breaking down glycogen into usable glucose, emerges as a key target. When researchers increased GlyP activity in animal models, they observed a significant reduction in glycogen accumulation and a corresponding decrease in neuronal damage. Such modulation not only improved cellular resilience but also extended lifespan in the tauopathy models, signaling a promising therapeutic avenue.
This enzyme-focused approach counters the fatalistic narrative that neurodegeneration is an inevitable consequence of aging. It suggests that boosting the brain’s intrinsic capacity to manage and dispose of glycogen may fortify neurons against the toxic effects of tau buildup and oxidative stress. Given that glycogen management can be influenced through dietary and pharmacological means, this discovery invigorates the pursuit of accessible, effective treatments.
Diet, Drugs, and the Future of Dementia Prevention
What’s particularly remarkable is that simple lifestyle modifications, such as dietary restriction, mimic the beneficial effects observed with direct enzyme activation. Experiments with low-protein diets in animal models on the verge of neurodegeneration demonstrated increased lifespan and reduced brain damage, reinforcing the idea that metabolic flexibility is a powerful tool in disease mitigation.
Furthermore, pharmaceutical efforts have already begun to tap into this insight. Researchers developed molecules, like 8-Br-cAMP, designed to replicate dietary benefits by stimulating glycogen breakdown pathways. These compounds showed promise in early tests, hinting at a future where drug regimens could complement or even replace lifestyle interventions. Notably, existing medications like GLP-1 receptor agonists—originally intended for diabetes management—may now have an expanded role in neuroprotection. These drugs potentially influence glycogen regulation pathways, offering hope that repurposing familiar medicines could accelerate the fight against dementia.
A Paradigm Shift with Powerful Implications
Fundamentally, this emerging narrative demands a reassessment of how we understand brain health and aging. Instead of viewing glycogen as a passive energy reserve, we should see it as a critical player in neuronal resilience and vulnerability. The potential to modulate glycogen metabolism through diet, drugs, or genetic interventions positions us at the cusp of a new era—one where neurodegenerative diseases are no longer seen as inevitable, but as conditions we can proactively influence by understanding and manipulating our brain’s internal chemistry.
The research underscores a broader truth: complex biological processes are rarely isolated, and energy balance within neurons might hold the key to unlocking therapies that can slow, halt, or even reverse cognitive decline. It challenges the neurodegeneration community to think beyond plaques and tangles and focus on the metabolic undercurrents that sustain or undermine brain vitality as we age. By shifting our gaze inward to the cell’s own chemistry, we open possibilities that could redefine the trajectory of Alzheimer’s and related diseases.
Leave a Reply