Axial spondyloarthritis (axSpA) is a chronic inflammatory condition that primarily affects the spine and sacroiliac joints, leading to significant pain and stiffness. This form of spondyloarthritis can manifest in two main ways: radiographic axSpA, often synonymous with ankylosing spondylitis, and non-radiographic axSpA, which may not present detectable changes on X-rays. Both types share similarities in symptoms and disease burden, but their management can vary significantly depending on patient response to treatment and the specific characteristics of the disease.
Individuals suffering from axSpA often experience debilitating symptoms that can severely impact their daily lives. The challenge lies not just in the physical discomfort but also in the potential for long-term structural changes that can result in permanent disabilities if not managed effectively. This reality underscores the importance of swift and appropriate treatment to mitigate pain and curb functional decline.
Current Treatment Strategies: Beyond NSAIDs
Traditionally, nonsteroidal anti-inflammatory drugs (NSAIDs) have been the first line of defense in managing axSpA symptoms. However, their effectiveness may not be universal; some patients either do not respond or are unable to tolerate these medications due to side effects. Consequently, the need for alternative therapeutic options has become a focal point in rheumatology.
Guidelines from reputable organizations, such as the Assessment of SpondyloArthritis International Society and the European League Against Rheumatism (ASAS-EULAR), stress the importance of a comprehensive treatment approach that combines pharmacological interventions with non-pharmacological methods, including lifestyle modifications, physical therapy, and patient education. This multidimensional strategy is vital for improving quality of life and maintaining functional abilities in axSpA patients.
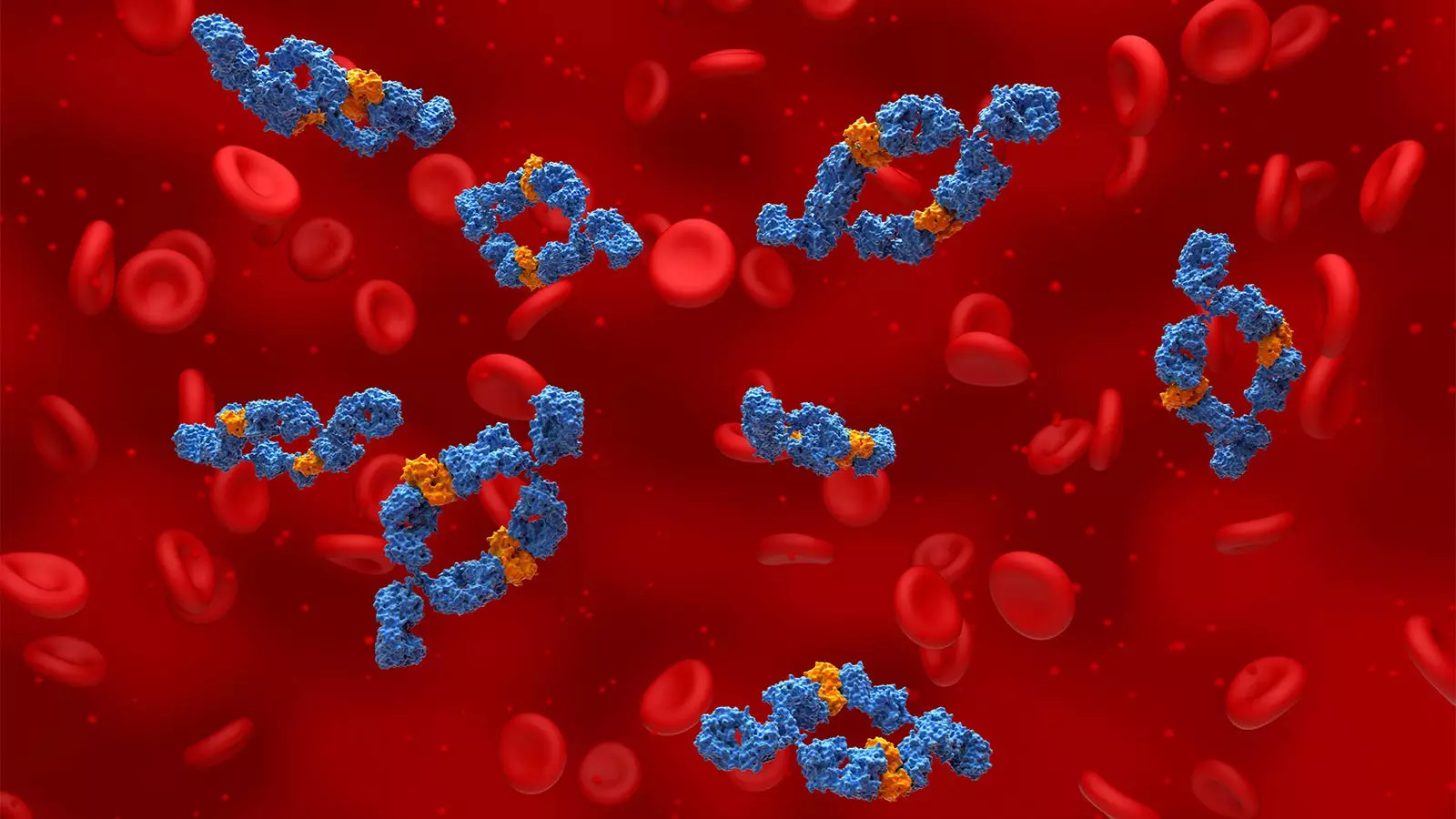
The introduction of biologic therapies has significantly transformed the treatment landscape for axSpA. These medications specifically target pathways involved in inflammation, offering new hope for patients who fail to achieve adequate relief with traditional NSAIDs. Among these biologic agents are tumor necrosis factor (TNF) inhibitors and interleukin (IL)-17 inhibitors. With the recent FDA approval of bimekizumab, an innovative IL-17A and IL-17F blocker, the therapeutic arsenal for managing axSpA has expanded further, providing options for different disease manifestations.
Bimekizumab’s approval in the United States and Europe marks a significant advancement, as clinical trials have demonstrated the drug’s efficacy across the spectrum of axSpA. Phase III studies such as BE-MOBILE 1 and BE-MOBILE 2 showed that a considerable proportion of patients experienced substantial improvement in their condition, confirming the role of targeting both IL-17A and IL-17F in achieving therapeutic goals.
Comparative Effectiveness: Navigating Treatment Choices
The rise of multiple biologic options begs the question of how to choose the most suitable treatment. Factors influencing this decision include the presence of extra-articular manifestations, response to previous therapies, and the patient’s cardiovascular profile. While TNF inhibitors like adalimumab and etanercept have been long-standing therapies, the introduction of IL-17 inhibitors and Janus kinase (JAK) inhibitors adds layers of complexity to treatment decisions.
Recent retrospective analyses comparing treatment outcomes shed light on the relative effectiveness and discontinuation rates associated with different therapies. Insights suggest that while TNF inhibitors might be more favored as front-line treatments due to their longstanding track record, JAK inhibitors could potentially lead to higher discontinuation rates, indicating that efficacy and safety profiles must be closely analyzed.
The future of axSpA management is undoubtedly dynamic, with ongoing research seeking to identify the most effective strategies for patient care. Continuous evaluation of biologic therapies, including longitudinal studies on bimekizumab, is essential to determine how best to tailor treatments for various patient populations. Additionally, understanding the nuances between similar agents and their individualized responses can help refine treatment approaches.
As new treatments become available, the rheumatology community remains committed to enhancing patient outcomes through a combination of innovative therapies and holistic management plans. In this new era of axSpA treatment, the aim is clear: to empower patients with the most effective options to improve their quality of life and manage their disease effectively.
Through persistent research and a focus on individualized care, there is hope for breakthroughs that will further enrich the available treatment landscape for axial spondyloarthritis, offering renewed hope to those affected by this challenging condition.
Leave a Reply