The approval of the Alzheimer’s drug lecanemab by the FDA in 2023 was hailed as a breakthrough in the treatment of a disease that ravages minds and tears families apart. The drug demonstrated an ability to slow cognitive decline by up to 27% in clinical trials, a glimmer of hope for millions. However, this promising statistic carries a rather troubling caveat—while this advancement may extend years of independence for some, it may not apply universally, especially across gender lines.
What’s alarming is that initial analyses suggest a staggering 31% difference in drug efficacy between male and female brains—an inequity that casts a long shadow over its approval. For a condition that primarily afflicts women, especially as they age—two-thirds of Alzheimer’s patients are female—this disparity begs for urgent scrutiny.
The Numbers Don’t Lie: Understanding the Gender Gap
As impressive as lecanemab’s results may sound, they only tell part of the story. Recent analyses, including simulations conducted in Canada and Italy, point to an unsettling reality: the effectiveness of the drug in women is, at best, limited. Through 10,000 simulated trials based on data from the original study, researchers uncovered that female patients demonstrated only a non-significant 12% mean slowing of cognitive decline. This distinction raises red flags, signaling that clinical trials are failing to encapsulate a complete understanding of how gender impacts drug responses.
Critics like neuroscientist Marina Lynch emphasize the historical negligence in considering sex differences within clinical trials. The lack of nuanced recruitment and reporting is not merely an oversight; it’s a systemic issue that needs rectification. By ignoring sex as a variable, we risk prescribing ineffective treatments to a significant portion of the population, which is not only unethical but also scientifically negligent.
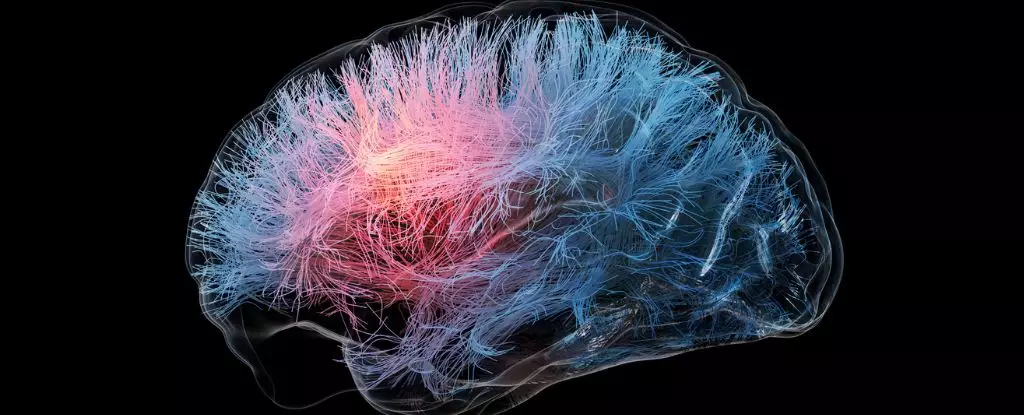
The Biological Maze: Amyloid Proteins and Cognitive Decline
The crux of lecanemab’s action hinges on targeting amyloid plaques in the brain—culpable agents often associated with Alzheimer’s. However, emerging research prompts us to question whether these plaques are the initial triggers of cognitive decline. Strikingly, current findings indicate that a considerable subset of individuals diagnosed with Alzheimer’s show no amyloid presence in postmortem examinations. This raises a critical dilemma: If these plaques aren’t the definitive cause, then why are we centering our treatments around them?
This pivot toward the drug’s mechanism has broader implications, particularly regarding gender. It’s plausible that sex hormones influence how amyloid forms in the brain and how effectively it’s cleared. Therefore, these gender disparities shouldn’t merely be viewed as statistical anomalies but as vital components that impact drug mechanisms and treatment efficacy.
A Call for Enhanced Research: The Need for Inclusivity
We are at a crucial juncture in neuroscience, and the data overwhelmingly suggest an urgent need for more gender-inclusive research. In 2019, only 5% of neuroscience studies engaged with the influence of sex on health outcomes. As experts warn, this male-centric focus not only perpetuates a knowledge gap but poses “grave consequences” for women’s health.
To combat this, there should be an industry-wide initiative to improve gender representation in clinical trials and subsequent analyses. A comprehensive understanding of why female brains age differently not only fosters equitable healthcare; it also builds a scaffolding for a more effective response to Alzheimer’s disease.
The Road Ahead: Moving Towards Equitable Solutions
Ignoring sex as a significant variable not only lengthens the timeline for medical advances but also exacerbates inequalities in healthcare. The path forward must embrace inclusivity and prioritize research that tackles these pressing gender disparities. Neuroscientists like Daniel Andrews emphasize the critical need for future work to link drug action mechanisms to sex differences in amyloid clearing and clinical outcomes.
The Alzheimer treatment landscape may be evolving, but without addressing these disparities, we risk further entrenching a system that favors male physiology over female health. As we advance toward clearer and more effective solutions, let us not merely celebrate advancements like lecanemab. Instead, let’s demand a paradigm shift that ensures all patients—regardless of sex—benefit from a therapeutic landscape designed with them in mind. The implications are not just academic; they are personal and profound.
Leave a Reply