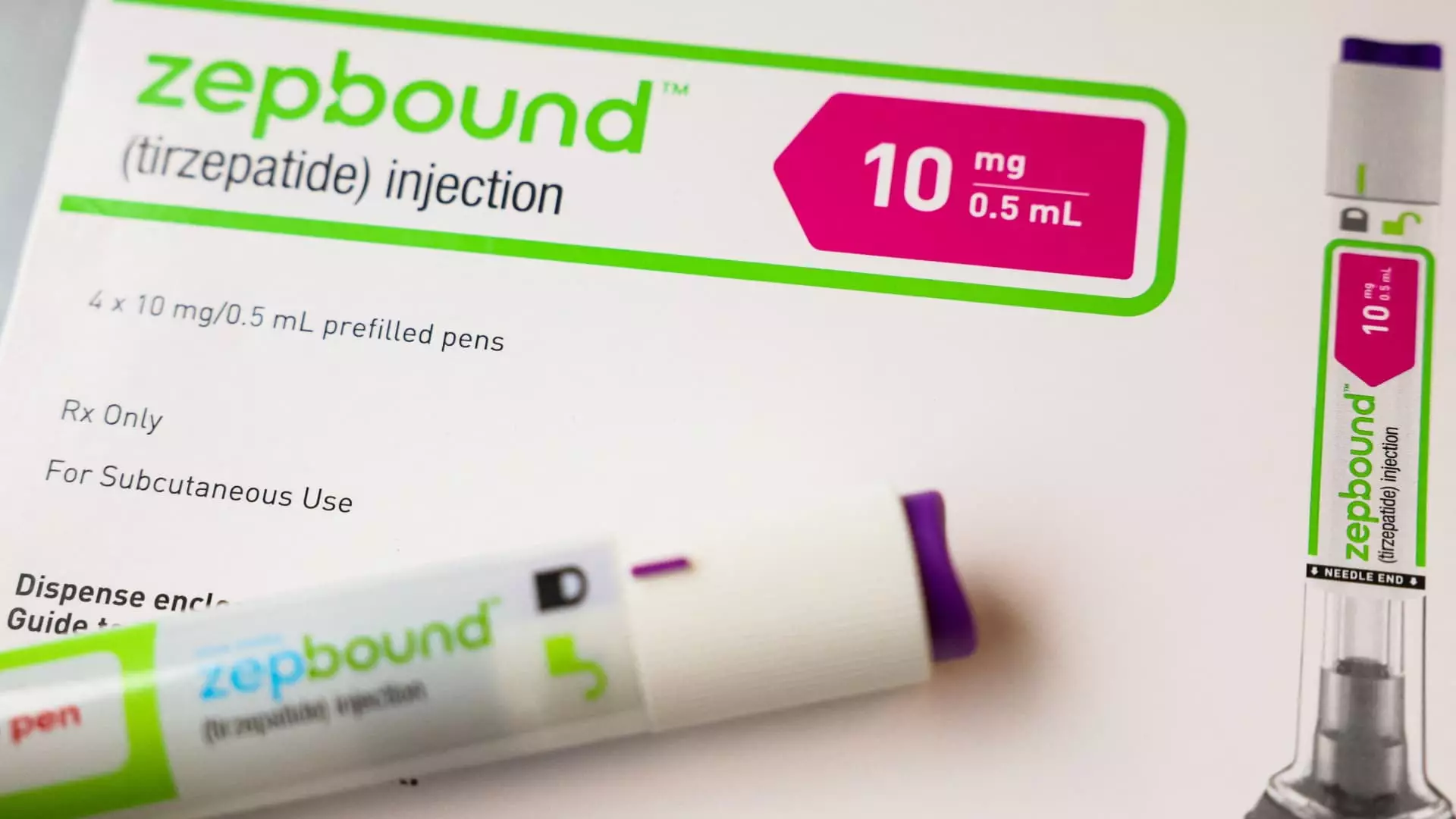
In a significant policy shift, Medicare drug plans have begun to include Eli Lilly’s groundbreaking obesity treatment, Zepbound, for patients with obstructive sleep apnea (OSA). This development, confirmed by CNBC, offers promising news for individuals suffering from obesity and sleep-related breathing disorders, allowing greater access to a medication that has recently gained attention for its effectiveness, despite its high price point. The implications of this inclusion not only alter the landscape of obesity treatment but could also affect public health outcomes as a whole.
Historically, Medicare has had stringent rules concerning the coverage of weight-loss medications, allowing them only in specific medical contexts that align with FDA approvals. The recent approval of Zepbound for OSA marks an important milestone, as it is the first medication specifically endorsed for treating a condition that affects an estimated 20 million Americans. Previously, Zepbound and similar medications were not covered under Medicare Part D, limiting access to those who could afford the out-of-pocket costs, which hover around $1,000 without insurance.
Obtaining Medicare coverage could lead to wider usage of Zepbound, making it a feasible option for many who were previously priced out of effective weight-loss treatments. However, the discussion around insurance coverage also highlights systemic issues regarding medication access based on specific health conditions.
Despite this positive development, the road to access is not entirely smooth. As clarified by a spokesperson from the Centers for Medicare & Medicaid Services (CMS), aspects like prior authorization may pose challenges. Providers will need to secure approval from insurers, which can delay access and create administrative burdens for both healthcare professionals and patients. This creates a layered complication where the drug’s approval does not automatically translate to ease of access, potentially dissuading healthcare providers from prescribing it or deterring patients from seeking it altogether.
Additionally, the statement mentioned that Medicare Part D plans are limited in their ability to cover obesity drugs unless they are utilized for a medically accepted purpose. While this opens the door for Zepbound, it simultaneously constrains how and when medical professionals can prescribe it, which may dissuade comprehensive treatment approaches.
The decision to include Zepbound in Medicare coverage is tied to larger conversations about healthcare spending and accessibility. The Biden administration previously suggested policy changes that would allow Medicare and Medicaid to broaden their coverage of weight-loss drugs, aiming to serve a wider population of patients with obesity. However, these measures could significantly increase taxpayer expenses, projected up to $35 billion over the next decade.
This intersection of access, cost, and healthcare policy raises critical questions on the societal approach to obesity—a complex health issue that is often stigmatized. Should the government extend greater coverage to obesity medications? Could this shift improve health outcomes for millions while also addressing long-standing health disparities? Alternatively, could it add undue strain on the healthcare system’s finances?
Pharmaceutical companies like Eli Lilly and Novo Nordisk are exploring various indications for their weight-loss drugs beyond obesity and sleep apnea, including chronic conditions like fatty liver disease and chronic kidney disease. However, before these drugs can be included in Medicare or Medicaid coverage for these uses, they must undergo rigorous late-stage clinical trials and secure FDA approvals.
The inclusion of Zepbound in Medicare drug plans signifies a potentially transformative movement in obesity care, raising hopes for enhanced access and improved health outcomes for millions. Yet, the surrounding complexities of insurance regulations, administrative hurdles, and broader policy ramifications must be carefully navigated to ensure that such advancements translate into meaningful benefits for the affected populations. As we foster discussions around obesity treatment, it is imperative to evaluate both the societal and individual implications of policy changes to promote equitable access to healthcare.
Leave a Reply