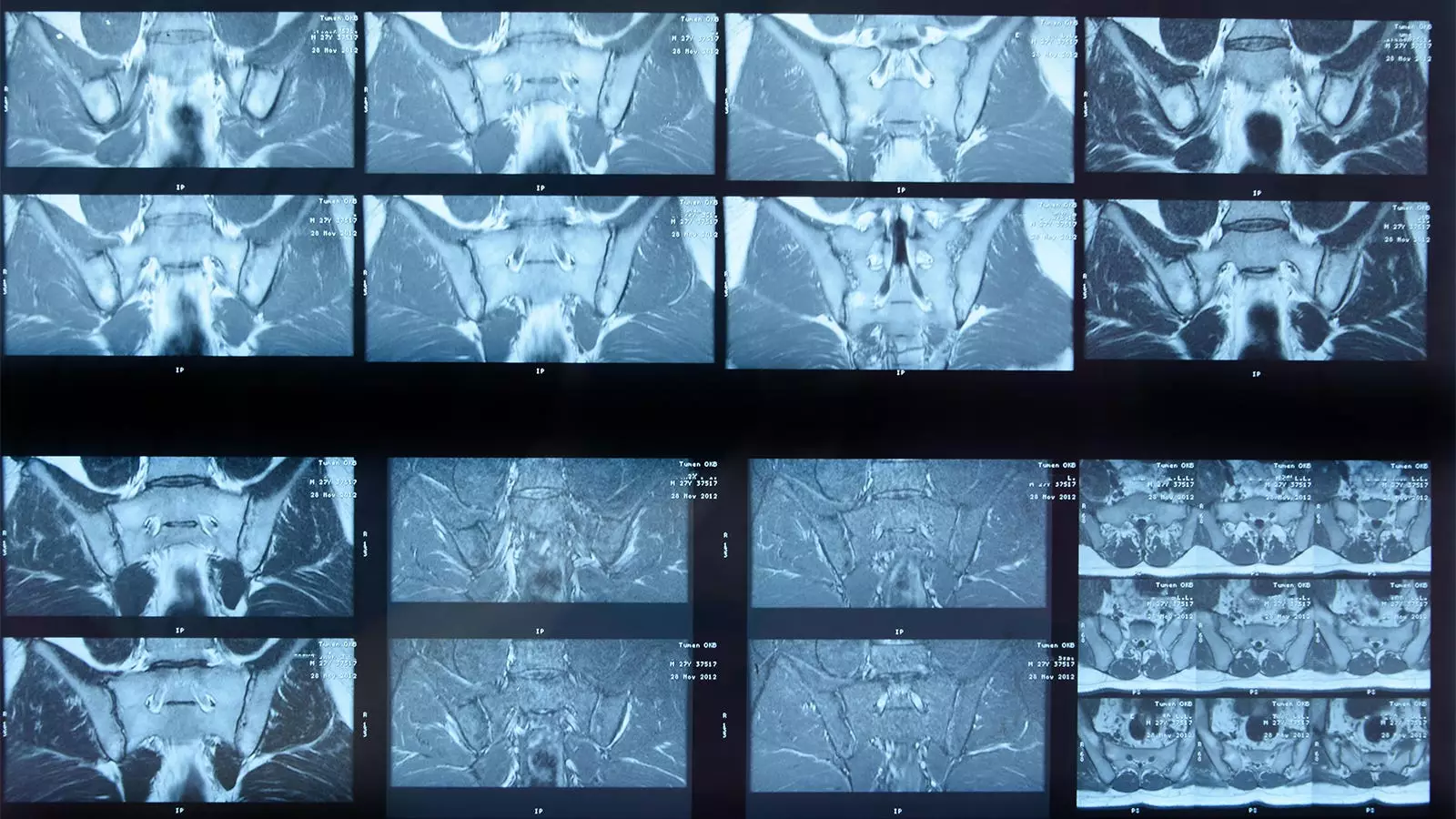
Artificial intelligence (AI) technology is increasingly penetrating various fields of healthcare, including radiology and the assessment of musculoskeletal disorders. A recent study by Joeri Nicolaes, PhD, and colleagues highlights the performance of a deep learning algorithm designed to analyze MRI scans for detecting sacroiliac joint (SIJ) inflammation specifically in patients suffering from axial spondyloarthritis (axSpA). While the researchers reported “acceptable” alignment with expert human readers, the findings reveal a complicated relationship between human expertise and machine learning algorithms in diagnostic settings.
The study presented a comparison between the deep learning algorithm’s assessments and those of a “gold standard” panel composed of three expert readers. Reviewing a total of 731 patient images, the AI demonstrated a notable level of concordance—achieving agreements on the presence of inflammation in 304 cases and the absence of inflammation in 239 cases. However, an essential concern arose as the algorithm missed inflamed SIJs in 132 cases, while falsely identifying inflammation in another 56 images that the expert readers deemed free of inflammation.
The researchers summarized the algorithm’s statistical performance, presenting metrics that include an absolute agreement rate of 74%, a sensitivity of 70%, and a specificity of 81%. Although these numbers might appear decent at first glance, they evoke serious inquiries regarding the algorithm’s effectiveness in real-world applications. For instance, a sensitivity score indicates the algorithm’s ability to identify true cases of inflammation, and a value of 70% suggests a significant rate of missed diagnoses. Furthermore, the algorithm’s negative predictive value of 64% raises questions about its reliability in reassuring clinicians when no inflammation is detected.
Nicolaes and his team acknowledged that the conservative criteria—for instance, the requirement for inflammation to be present in at least two SIJs—might have adversely influenced these figures. They suggested that the expert readers’ access to contextual information, such as clinical biomarkers like C-reactive protein (CRP) levels or HLA-B27 positivity, likely enhanced their diagnostic accuracy beyond what the algorithm could achieve. This raises an essential issue: the necessity of integrating clinical information with machine-driven assessments to improve diagnostic outcomes.
A significant concern highlighted in the study is the varying expertise among human readers, which can lead to inconsistent interpretations. While the panel of experts may have included some of the best in the field, many rheumatologists and radiologists managing these cases in clinical practice may not have similar expertise. In this context, the algorithm could serve as a valuable adjunct—providing consistent results that may reduce variability in human interpretation. The researchers optimistically concluded that such algorithms could potentially fill gaps in settings where expert readers are scarce, yet the limitations of the algorithm itself cannot be understated.
One of the key insights of the study was the reflection upon the evolving nature of imaging classification criteria. The current standards concerning SIJ inflammation have changed since the algorithm was designed. This necessitates future refinements to algorithms like the one in question to ensure alignment with contemporary practices. Moreover, the absence of functionality that could detect structural damage from the scans limits the current algorithm’s applicability in assisting treatment planning.
The study signifies a critical moment for the intertwining of AI and clinical practice in the field of musculoskeletal diseases. While the AI algorithm demonstrated promising outcomes, especially in terms of reproducibility, the effectiveness and reliability inherent in its performance warrant cautious optimism. The healthcare community must critically examine how such technologies can complement human expertise rather than replace it.
This blend of human diagnostic skill and artificial intelligence could herald a new era of medical imaging where the strengths of each converge. Future research should not only focus on enhancing algorithmic performance but also explore integrating broader clinical data inputs to improve diagnostic accuracy. Ultimately, forging a pathway where AI and human insight collaborate could significantly change the landscape of diagnosing and managing axial spondyloarthritis, leading to better patient outcomes.
Leave a Reply