As individuals progress through life, the brain faces a daunting challenge: an inevitable decline in its essential cleaning processes that are crucial for maintaining cognitive functions. This deterioration leads many to confront the threatening prognosis associated with age-related neurodegenerative diseases like Alzheimer’s. Recent research led by Washington University in St. Louis provides a beacon of hope, revealing that targeted therapies aimed at enhancing the brain’s waste management systems may not only combat memory decline but could significantly alter the landscape of how we approach aging and cognitive health.
The Role of Meningeal Lymphatics: Unsung Heroes of Brain Health
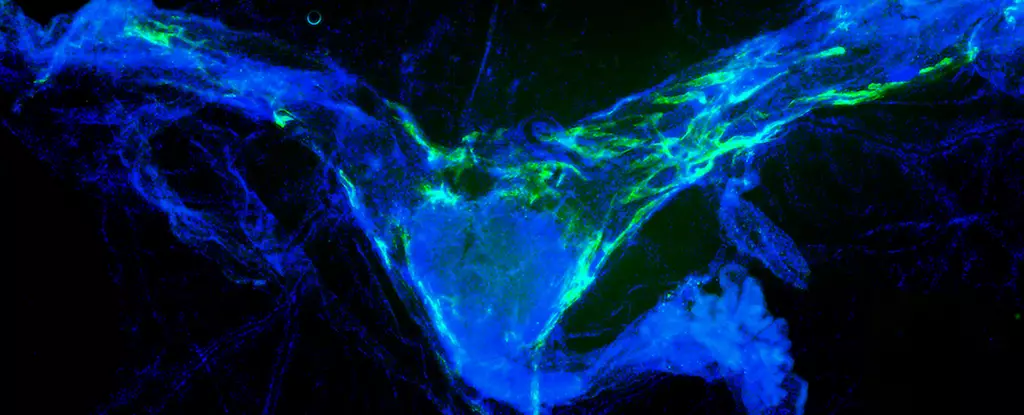
Central to this innovative research is a focus on the meningeal lymphatic vessels—structures frequently overlooked yet vital for cognitive vitality. These channels form part of the body’s comprehensive lymphatic system responsible for waste removal and immune function. Incredibly, the study concluded that boosting the function of these vessels in older mice led to remarkable improvements in memory. This finding underscores the importance of maintaining a functional lymphatic system, particularly as it pertains to optimizing brain health in the aging population.
This research raises critical questions about our current understanding of cognitive health maintenance. Could interventions focusing on these lymphatic pathways provide a healthier alternative to traditional therapies that often rely heavily on pharmacological approaches? The answer may lie in continuing to explore how these vessels can be manipulated for therapeutic benefits.
Insights into Microglial Response and Cognitive Maintenance
Beyond the surface findings, the research provides deep insights into the relationship between the immune system and cognitive function. In instances when brain waste management falters, microglial cells—key players in the immune response—begin to exhibit distress, emitting signals such as interleukin 6 to denote their overwhelmed state. Such responses create a vicious cycle, where inflammation exacerbates cognitive decline, further complicating the brain’s ability to perform its necessary tasks.
However, the interventions implemented in the studies not only improved memory but also reduced levels of interleukin 6, effectively crescendoing a beneficial cycle that restores order to immune functions. The consequences of this discovery could be transformative, suggesting a pathway to prevent damage often seen in aging brains through targeted lymphatic enhancements.
Strategic Targeting: A Paradigm Shift in Neurological Therapies
One striking advantage of this research is the viability of targeting meningeal lymphatic vessels, which reside conveniently outside the blood-brain barrier. This innovation circumvents a long-standing hurdle in neuroscience: how to deliver effective therapies without the complications posed by this layer of protective tissue. By approaching treatment from a different angle—through the lymphatics—scientists may unlock more powerful therapeutic applications that hold the potential to delay or prevent cognitive decline.
As Jonathan Kipnis notes, circumventing the challenges posed by the blood-brain barrier opens the door to developing therapies that could offer substantial cognitive benefits without the multifactorial challenges typical of traditional methods. This approach not only provides tangible hypotheses for future study but inscribes a new paradigm in how we perceive the interactions between the brain and its immune support systems.
Connecting Previous Research: Building a Cohesive Understanding
The findings are particularly insightful when viewed in the context of prior studies, such as the 2022 investigation that showed enhancement of memory via cerebrospinal fluid injections. This correlation reinforces the understanding that optimal brain function is contingent upon effective waste clearance mechanisms, akin to preventing congestion on a train track. The capacity to ensure ongoing cognitive function may not reside solely in reviving neurons but rather in maintaining an optimal environment for these cells to thrive.
This emerging perspective champions the notion that cognitive health in the aging population may hinge more on support systems—like the meningeal lymphatics—rather than solely on neuron activity. This shift could herald significant changes in therapeutic strategies aimed at slow cognitive decline and cultivate a more holistic view of brain health.
By bravely investigating the brain’s cleanup crew, researchers have not only highlighted the critical links between lymphatic function and cognitive health but have also provided a framework for discovery that could redefine our approach to aging and memory resilience.
Leave a Reply