In recent years, the link between dietary habits and cognitive health has become a focal point of research, especially among older adults. A growing body of evidence suggests that diets high in inflammatory foods may increase the risk of developing dementia, including Alzheimer’s disease. The Framingham Heart Study Offspring cohort has provided substantial insights into this relationship, indicating that long-term consumption of certain foods directly correlates with the incidence of dementia.
The study in question utilized the Dietary Inflammatory Index (DII), a scoring system that evaluates the inflammatory potential of diets based on food intake. By examining data from 1,487 participants over a 13-year span, researchers reported significant findings regarding the relationship between DII scores and the incidence of dementia. High DII scores, indicative of an inflammation-promoting diet, were positively associated with the development of all-cause dementia, with a hazard ratio suggesting a 21% increased risk. Similarly, higher scores were associated with a 20% increased risk for Alzheimer’s dementia, raising red flags for health experts aiming to mitigate cognitive decline in the aging population.
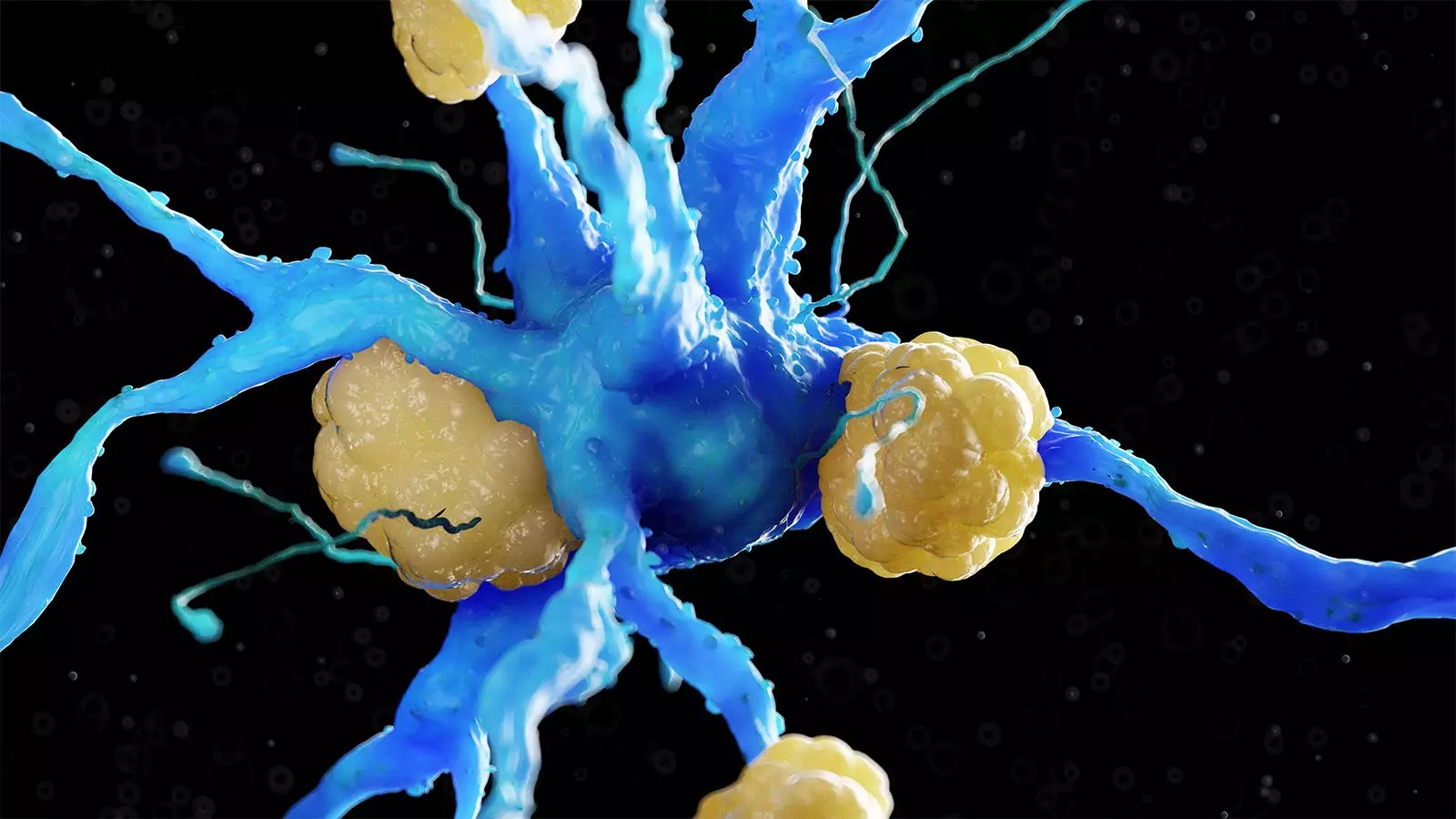
At the heart of these findings lies the concept of inflammation, which has been implicated in a multitude of health issues, including neurodegenerative diseases. Inflammatory foods, often found in a typical Western diet, include excessive saturated and trans fats, refined carbohydrates, and added sugars. Such dietary patterns are not only linked to systemic inflammation but have also been associated with negative brain outcomes, such as reduced gray matter volume and increased lateral ventricular size.
Interestingly, this study aligns with previous research asserting that dietary choices significantly affect brain health. The MIND diet — a fusion of Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets — has been noted for its potential cognitive benefits by emphasizing anti-inflammatory foods. This diet has demonstrated a similar ability to preserve cognitive function over time, highlighting the importance of dietary interventions in promoting brain health.
The robustness of the Framingham Heart Study is underscored by its longitudinal design and comprehensive data collection methods. The 126-item Harvard food frequency questionnaire was employed to gather dietary information at three distinct time points spanning a decade. This meticulous approach allowed researchers to average DII scores, providing a clearer picture of participants’ dietary patterns.
Participants in this study were predominantly older adults, averaging 69 years of age, with a diverse demographic profile. It is noteworthy that about 22% of the cohort carried the APOE4 allele, a genetic marker known to amplify Alzheimer’s disease risk. Researchers meticulously adjusted findings for various demographic, lifestyle, and clinical covariates, thus reinforcing the credibility of their conclusions.
The implications of this research are profound. With dementia rates on the rise globally, understanding risk factors, particularly modifiable ones like diet, is crucial for public health strategies aimed at prevention. The study’s authors advocate for dietary interventions prioritizing anti-inflammatory foods as potential protective measures against neurodegenerative diseases.
However, while the findings are promising, they do come with limitations. The observational nature of the study does not allow for conclusions regarding causality, and reliance on food frequency questionnaires poses challenges in accuracy. Furthermore, the inability to assess all possible DII components raises questions about the completeness of the dietary analysis. As researchers noted, some dietary components may influence health outcomes differently than expected, which complicates interpretations of data.
Future research must build upon these foundational findings by exploring the long-term causal relationship between diet-driven inflammation and cognitive health. More targeted studies should focus on broader dietary patterns and their contributions to dementia prevention or progression. Additionally, clinical trials could examine the efficacy of specific anti-inflammatory diets, such as the MIND diet or Mediterranean diet, to elucidate their roles in cognitive health maintenance among aging adults.
Moreover, educating the public about the risks associated with inflammatory diets and promoting anti-inflammatory alternatives could serve as effective strategies in community health initiatives. As the scientific community continues to unravel the complexities of diet and dementia, the hope is that actionable dietary guidelines can emerge, empowering individuals to take charge of their cognitive health as they age.
The Framingham Heart Study highlights a pressing need for awareness and action regarding dietary choices as we advance into an era increasingly fraught with cognitive health challenges.
Leave a Reply